Overview
There are common symptoms of optic neuritis, which include pain with eye movement and temporary vision loss in one eye. Optic neuritis is caused by swelling (inflammation) that damages the optic nerve.
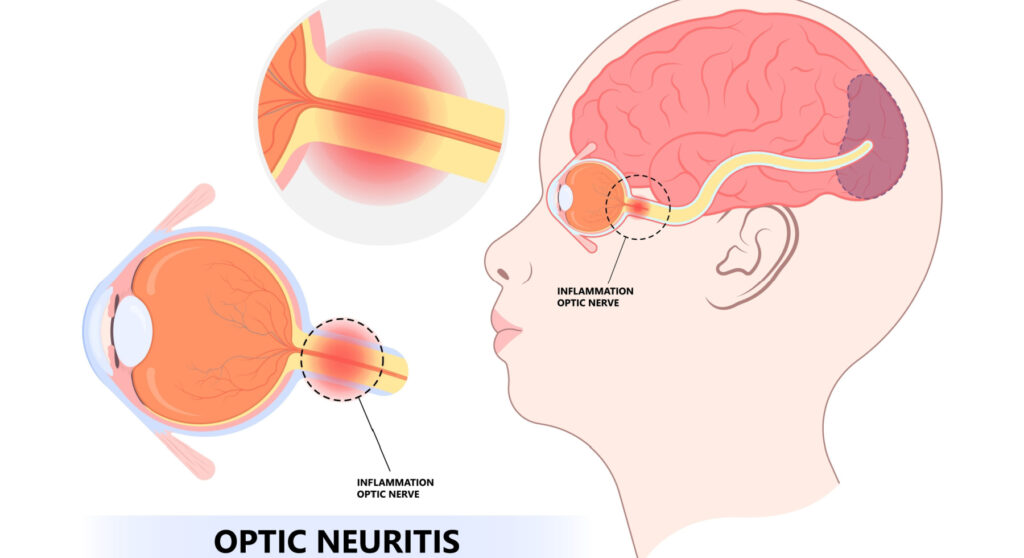
Optic nerve
Optic nerves are bundles of nerve fibers which serve as a communication channel between the eyes and the brain. The fibers are coated with a material known as myelin to ensure that they function properly.
MS is a disease which causes inflammation and damage to nerves in the brain and to the optic nerve. Symptoms of optic neuritis may be the first sign of MS, or they may appear later in the course of MS.
There are several other conditions that can cause inflammation of the optic nerve and spinal cord, including infections or immune diseases such as lupus. In rare cases, another disease called neuromyelitis optica can also cause inflammation.
The majority of patients who experience a single episode of optic neuritis eventually recover their vision without treatment. In some instances, steroid medications may help to speed up the recovery of vision.
Symptoms
A person suffering from optic neuritis usually experiences symptoms in one eye. These symptoms may include:
-
The pain that most people experience when they develop optic neuritis is worsened by eye movement. Sometimes the pain feels like a dull ache in the area behind the eye.
-
The loss of vision in one eye is common. Most people have some temporary vision loss, but the extent of the loss varies. Visual loss usually occurs in an eye over a period of hours or days and improves over a period of weeks or months.
-
Loss of visual field. Loss of side vision can occur in any pattern, including central and peripheral vision loss.
-
The loss of color vision that is often associated with optic neuritis. You may notice that colors appear less vivid than they normally do.
-
A flashing or flickering light may be seen by some people with optic neuritis when they move their eyes.
When to see a doctor
The following conditions can be serious. Some can result in permanent vision loss, while others are associated with other serious medical conditions. Please consult your doctor if you are experiencing the following symptoms:
-
A new symptom arises, such as eye pain or a change in vision.
-
Symptoms do not improve or worsen as a result of treatment.
-
There are unusual symptoms, such as double vision, vision loss in both eyes, and numbness or weakness in one or more limbs, which can indicate a neurological disorder.
The causes
Optic neuritis is a condition that occurs when the immune system mistakesnly targets the substance that covers your optic nerve, resulting in inflammation and damage to the myelin covering it. The exact cause of optic neuritis is unknown.
Myelin normally facilitates the rapid transmission of electrical impulses from the eye to the brain, where they are converted into visual information. Optic neuritis causes this process to be disrupted resulting in poor vision.
There are several autoimmune conditions that are often associated with optic neuritis, including:
-
Multiple sclerosis is a condition in which the immune system attacks the myelin sheath covering the nerve fibers in the brain and results in multiple sclerosis. Approximately 50% of people with optic neuritis will develop multiple sclerosis after one episode of optic neuritis.
If an MRI scan reveals brain lesions following optic neuritis, your risk of developing multiple sclerosis increases further.
-
Neuromyelitis optica. This condition involves inflammation of the optic nerve and spinal cord. Unlike multiple sclerosis, neuromyelitis optica does not cause as much damage to brain nerves as multiple sclerosis. In addition, neuromyelitis optica has a higher severity than MS, often resulting in diminished recovery following attacks.
-
The MOG antibody disorder causes inflammation of the optic nerve, spinal cord, or brain. It is similar to MS and neuromyelitis optica, where recurrent attacks of inflammation can occur. Myelin oligodendrocyte glycoprotein (MOG) attacks are generally more easily recovered from than neuromyelitis optica attacks.
It is important to consider other associated causes of optic neuritis when symptoms of optic neuritis are more complex, including:
-
Bacterial infections, such as Lyme disease, cat scratch fever, and syphilis, as well as viral infections, such as measles, mumps, and herpes, may cause optic neuritis.
-
A number of other diseases can cause recurrent optic neuritis, such as sarcoidosis, Behcet’s disease, and lupus.
-
Toxins and drugs have also been associated with optic neuritis, for example, ethymbutol, a drug used to treat tuberculosis, and methanol, a chemical used to make antifreeze, paints, and solvents.
Risk factors
The following factors increase the risk of developing optic neuritis:
-
It is most common among adults between the ages of 20 and 40 to suffer from optic neuritis.
-
The incidence of optic neuritis is much higher among women than among men.
-
The incidence of optic neuritis is higher in whites.
-
Various genetic mutations have been linked to a higher risk of optic neuritis and multiple sclerosis.
Complications
Optic neuritis may result in the following complications:
-
Optic nerve damage. Most people have some permanent optic nerve damage after an episode of optic neuritis, but the damage might not cause permanent symptoms.
-
A reduction in visual acuity. Most people regain normal or near-normal vision within several months, but a partial loss of color discrimination may persist. Vision loss may persist for some people.
-
Steroid medications for the treatment of optic neuritis suppress the immune system, causing your body to be more susceptible to infection. Other side effects include mood changes and weight gain.